A CASE OF CHRONIC RENAL FAILURE PRESENTED IN SUMMER 2022
NOTE:
- The following E-log aims at discussing our patient de-identified health data shared after taking the guardian's signed consent.
- Here we discuss our individual patient problems through series of inputs from available global online community of experts with an aim to solve the patients clinical problem with current best evidence based input.
- This E-log also reflects my patient's centered online learning portfolio.
- I have been given this case to solve in an attempt to understand the topic of "Patient Clinical Data Analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and providing treatment best to our skills and wisdom.
A 65 years old lady farmer by occupation presented in the casualty with complaints of shortness of breath and pedal edema.
CHIEF COMPLAINTs
➤SOB for last 4 days
➤Cough for last 4 days
➤Pain in lower limb for last 4 days
HISTORY OF PRESENTING ILLNESS
Patient was apparently asymptomatic 4 months back. In April , She had SOB on exertion with tingling sensation in both upper and lower arms, pedal edema and decrease in urine output ( creatinine : 3.1mg/dl )for which she got treated in nearby hospital and her symptoms got resolved. Again by end of June She had nausea , vomiting ,weakness ,burning micturition and pain in lower limb (creatinine : 3.8mg/dl uric acid:5.6mg/dl) for which she was treated and all her complains got resolved .In July she presented with pain in lower limbs ( creatinine : 5.2mg/dl uric acid:6.4mg/dl)for which she got treated and symptoms got resolved.
In mid of august she came to our hospital with complaints of SOB for past 4 days which is of grade II . It is associated with cough with expectorant. She is also having pain in both lower limb from knee to toes only on movement for past 4 days. Pain is of non radiating type. She works as a cotton picker and experience pain even in bending down to pick cottons.No redness and tenderness present at or around joints.Not having feverNo abdominal painNo back ache.
HISTORY OF PAST ILLNESS ➤Not a known case of diabetes ,bronchial asthma ,epilepsy, tuberculosis
➤k/c/o hypertension for 8 years
DRUG HISTORY
➤Tab Atenolol 50mg OD for HTN for last 8 years
PERSONAL HISTORY
➤ Occupation : Farmer
➤Patient is married
➤Patient takes mixed diet but has a decreased appetite.
➤Bowel and bladder movement is normal and regular.
➤No addiction
FAMILY HISTORY
➤No significant family history.
GENERAL EXAMINATION
➤Pallor :Not seen
➤Icterus : Not seen
➤Cyanosis : Not seen
➤Clubbing : Not seen
➤Lymphadenopathy : Not seen
➤Edema : Not seen
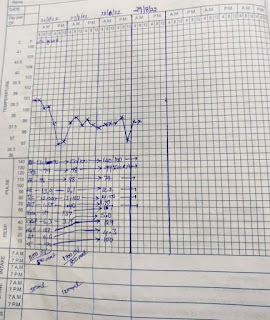
VITALS
➤Temperature : 98.3℉
➤PR : 76 beats per minute
➤BP : 130/80 mm of Hg
➤RR : 18 cycles per minute
➤SpO2 : 97% in room air
➤Blood Sugar (random) : 119mg/dl
SYSTEMIC EXAMINATION
CARDIOVASCULAR SYSTEM EXAMINATION
➤s1 and s2 heard
➤Thrills absent.,
➤No cardiac murmurs
RESPIRATORY SYSTEM
➤Normal vesicular breath sounds heard.
➤Bilateral air entry present
➤Trachea is in midline
ABDOMINAL EXAMINATION
INSPECTION
➤Shape - Scaphoid
➤Equal movements in all the quadrants.
➤No visible pulsation, dilated veins and localized swellings.
PALPATION
➤No tenderness
➤No palpable mass
CENTRAL NERVOUS SYSTEM EXAMINATION
➤Conscious and coherent
PROVISIONAL DIAGNOSIS : CHRONIC RENAL FAILUE
DAY 1
INVESTIGATIONS :
1) COMPLETE BLOOD PICTURE
2) RFT

BLOOD UREA 158 mg/dl

CREATININE 6.2 mg/dl
3)USG ABDOMEN
4) SERUM IRON 73ug/dl
TREATMENT
1) TAB. NICARDIA PO/OD
2)TAB NODOSIS
3)TAB SHELCAL 500mg PO/OD
4)TAB OROFER XT PO/OD
5)CAP BI0 D3 PO/OD WEEKLY ONCE
6)INJ. ERYTHROOIETIN 4000IU S/C TWICE WEEKLY
7)INJ. PANTOP 40MG
8)INJ.ZOFER
DAY 2TREATMENT
1) TAB. NICARDIA PO/OD
2)TAB NODOSIS
3)TAB SHELCAL 500mg PO/OD
4)TAB OROFER XT PO/OD
5)CAP BI0 D3 PO/OD WEEKLY ONCE
6)INJ. ERYTHROOIETIN 4000IU S/C TWICE WEEKLY
7)INJ. PANTOP 40MG
8)INJ.ZOFER
DAY 3TREATMENT
1) TAB. NICARDIA PO/OD
2)TAB NODOSIS
3)TAB SHELCAL 500mg PO/OD
4)TAB OROFER XT PO/OD
5)INJ. ERYTHROOIETIN 4000IU S/C TWICE WEEKLY
Dialysis started at 10 pm & ended at 12 am
Weight loss-500gm
➤Not a known case of diabetes ,bronchial asthma ,epilepsy, tuberculosis
➤k/c/o hypertension for 8 years
DRUG HISTORY
➤Tab Atenolol 50mg OD for HTN for last 8 years
PERSONAL HISTORY
➤ Occupation : Farmer
➤Patient is married
➤Patient takes mixed diet but has a decreased appetite.
➤Bowel and bladder movement is normal and regular.
➤No addiction
FAMILY HISTORY
➤No significant family history.
GENERAL EXAMINATION
➤Pallor :Not seen
➤Icterus : Not seen
➤Cyanosis : Not seen
➤Clubbing : Not seen
➤Lymphadenopathy : Not seen
➤Edema : Not seen
VITALS
➤Temperature : 98.3℉
➤PR : 76 beats per minute
➤BP : 130/80 mm of Hg
➤RR : 18 cycles per minute
➤SpO2 : 97% in room air
➤Blood Sugar (random) : 119mg/dl
SYSTEMIC EXAMINATION
CARDIOVASCULAR SYSTEM EXAMINATION
➤s1 and s2 heard
➤Thrills absent.,
➤No cardiac murmurs
RESPIRATORY SYSTEM
➤Normal vesicular breath sounds heard.
➤Bilateral air entry present
➤Trachea is in midline
ABDOMINAL EXAMINATION
INSPECTION
➤Shape - Scaphoid
➤Equal movements in all the quadrants.
➤No visible pulsation, dilated veins and localized swellings.
PALPATION
➤No tenderness
➤No palpable mass
CENTRAL NERVOUS SYSTEM EXAMINATION
➤Conscious and coherent
PROVISIONAL DIAGNOSIS : CHRONIC RENAL FAILUE
DAY 1
INVESTIGATIONS :
1) COMPLETE BLOOD PICTURE
2) RFT
 |
| BLOOD UREA 158 mg/dl |
 |
| CREATININE 6.2 mg/dl |
TREATMENT
1) TAB. NICARDIA PO/OD
2)TAB NODOSIS
3)TAB SHELCAL 500mg PO/OD
4)TAB OROFER XT PO/OD
5)CAP BI0 D3 PO/OD WEEKLY ONCE
6)INJ. ERYTHROOIETIN 4000IU S/C TWICE WEEKLY
7)INJ. PANTOP 40MG
8)INJ.ZOFER
TREATMENT
1) TAB. NICARDIA PO/OD
2)TAB NODOSIS
3)TAB SHELCAL 500mg PO/OD
4)TAB OROFER XT PO/OD
5)CAP BI0 D3 PO/OD WEEKLY ONCE
6)INJ. ERYTHROOIETIN 4000IU S/C TWICE WEEKLY
7)INJ. PANTOP 40MG
8)INJ.ZOFER
TREATMENT
1) TAB. NICARDIA PO/OD
2)TAB NODOSIS
3)TAB SHELCAL 500mg PO/OD
4)TAB OROFER XT PO/OD
5)INJ. ERYTHROOIETIN 4000IU S/C TWICE WEEKLY
Dialysis started at 10 pm & ended at 12 am
Weight loss-500gm



Comments
Post a Comment