A CASE OF 48 YEAR OLD MALE WITH CIDP
Log also reflects my patient's center ed online learning portfolio.
I have been given this case to solve in an attempt to understand the topic of "Patient Clinical Data Analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and providing treatment best to our skills and wisdom.
A 48yr old patient , resident of Chintapally, farmer by profession , presented to the casualty with complaints of weakness of both lower limbs and burning sensation in the feet .
Date of Admission: 04/06/23
CHIEF COMPLAINTS
➤ Weakness of both lower limbs since 6 months .
➤ Burning sensation in feet since 1 month .
HISTORY OF PRESENTING ILLNESS
Patient was apparently asymptomatic 6 months back .
Then he developed weakness in both lower limbs - it was insidious in onset and gradually progressed. It was associated with pain in the calf muscle .
He then developed burning sensation in his foot 1 month back , associated with tingling which can't be appreciated due to burning sensation.
He was able to walk on his own untill 1 month ago , but since then he needs support.
Patient complains of weight loss since 1 month .
Patient complains of losing footwear while walking.
He visited local hospital 6 months back and has been taking medication since then
HISTORY OF PAST ILLNESS
➤Not a K/c/o diabetes, hypertension, asthma , epilepsy tuberculosis , CAD
➤No surgical history
➤No history of Blood transfusions.
PERSONAL HISTORY
➤Occupation: Farmer.
➤Patient is married .
➤Patient takes mixed diet and has a normal appetite currently. He had decreased appetite 1 month back .
➤Sleep : Regular
➤Bowel and bladder movements are normal
➤No known allergies .
➤ Addictions: He had a history of taking alcohol since 25 years and stopped one year back.
GENERAL EXAMINATION
➤ Patient is conscious,coherent , cooperative well known with time, place, person
➤ He is well built and moderately nourish
➤Pallor : not seen
➤Icterus : not seen
➤Cyanosis : not seen
➤Clubbing : not seen
➤Lymphadenopathy : not seen
➤Edema : not seen
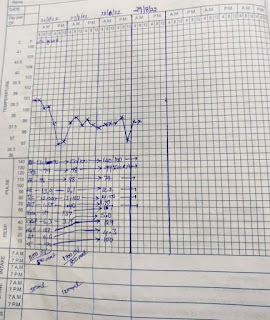
VITALS
Afebrile
PR- 94bpm
BP- 100/90mmHg
RR- 14cpm
SYSTEMIC EXAMINATION
CARDIOVASCULAR SYSTEM EXAMINATION
➤s1 and s2 heard
➤Thrills absent.,
➤No cardiac murmurs
RESPIRATORY SYSTEM
➤Normal vesicular breath sounds heard.
➤Bilateral air entry present
➤Trachea is in midline.
ABDOMINAL EXAMINATION
INSPECTION
➤Shape - Scaphoid
➤Equal movements in all the quadrants.
➤No visible pulsation, dilated veins and localized swellings.
PALPATION
➤Liver , spleen not palpable.
➤No tenderness
CENTRAL NERVOUS SYSTEM EXAMINATION
➤Conscious and coherent
➤Speech : Normal
➤No signs of meningeal irritation
➤Cranial Nerves - intact
➤ Glascow Scale - 15/15
Neck stiffness: no
Kernig's sign : no
Tone : UL. LL
Rt. Normal normal
Lf. Normal. Normal
Gait - High stepping
Power of right and left UL and LL is
5/5 and 4/5
Reflexes. B T. S. K. A. plantar
Lt: 2+. 2+. +. 3+. -.M
Rt: 2+. 2+. +. 3+. -. M
PROVISIONAL DIAGNOSIS : CHRONIC INFLAMMATORY DEMYELINATING POLYNEUROPATHY .
INVESTIGATIONS:
ECG:
CBP:
CUE:
USG:
1) Optineuron injection 1 amp 100 ml NS/IV BD
2)Tab Pregabalin 75 mg po /hs
3)Tab Ecosporin Av 75/10 po/ hs
4) Tab pan 40mg PO / OD.





Comments
Post a Comment